A cesarean scar defect is a complication that arises as a long-term consequence of a cesarean section. When women undergo a cesarean section, an incision is made inside the uterus to facilitate the baby’s delivery. Sometimes, this incision doesn’t heal completely, leaving a small opening inside the uterus where fluid can accumulate. This opening in the uterine wall is known as a cesarean scar defect or a “niche.”
A recent study involving nearly 2,500 women found that 60% to 70% had a niche following a cesarean section. Such a high occurrence makes one wonder if it’s not “normal” to have a niche. About 30% of these women have a “large” niche. To put this in perspective, the wall of the uterus is between 8 and 10 millimetres and a niche is called large when it’s bigger than half of the thickness. In other words, even a “large niche” is usually only 5-6 mm big.
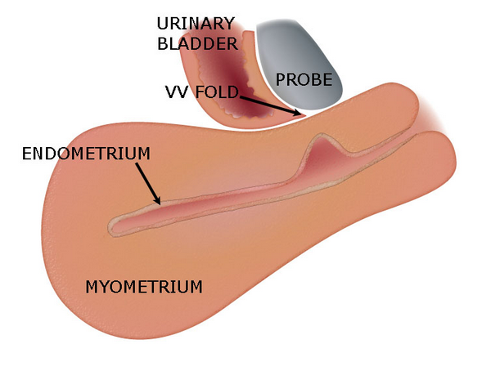
Detecting a niche can sometimes be straightforward, especially if a significant amount of fluid is present, making it visible via ultrasound. However, its appearance might be subtle at times, necessitating the introduction of gel or water into the uterus to highlight the defect. The amount of fluid in the niche can also vary depending on where a woman is in her menstrual cycle, which means it can sometimes be overlooked in ultrasounds, particularly if the gynaecologist isn’t specifically trained to spot it.
Niches can also cause symptoms, which I will discuss in this blog post. So, if you’ve had a cesarean section and begin experiencing related symptoms afterwards, requesting a detailed ultrasound is a good idea. We’ve recently coined a term for this combination of a niche and complaints: “cesarean scar disorder.” Defined in 2023, this disorder has garnered significant media attention, which is positive. We truly believe it’s essential for women to understand that one of the long-term complications of a cesarean scar can lead to this disorder.
Cesarean scar disorder is typically diagnosed through a combination of ultrasound detection of a niche and symptoms like intermittent bleeding, pain during menstruation, or challenges with fertility. Primary symptoms are directly linked to the scar defect, and secondary symptoms often arise due to the primary ones. For instance, some women report an unpleasant odour, likely due to intermittent bleeding. Others may feel less hygienic and subsequently avoid sexual intimacy or struggle with infertility.
By itself, a cesarean scar defect isn’t necessarily problematic. However, cesarean scar disorder can be concerning and warrants a diagnosis and potential treatment. While I won’t delve into treatment options in this post, various methods are available. It’s crucial to remember that many women with a cesarean scar don’t experience the disorder, and among those who do, not all require treatment.
As of 2023, we’ve outlined the disorder’s criteria and diagnostic techniques, and we’re actively exploring optimal treatment methods to assist women facing this issue. If you believe you might have cesarean scar disorder, I’d recommend seeking expert advice.